Kingston University psychology expert warns of emotional challenges facing NHS healthcare professionals working in intensive care units
Posted Monday 24 April 2017
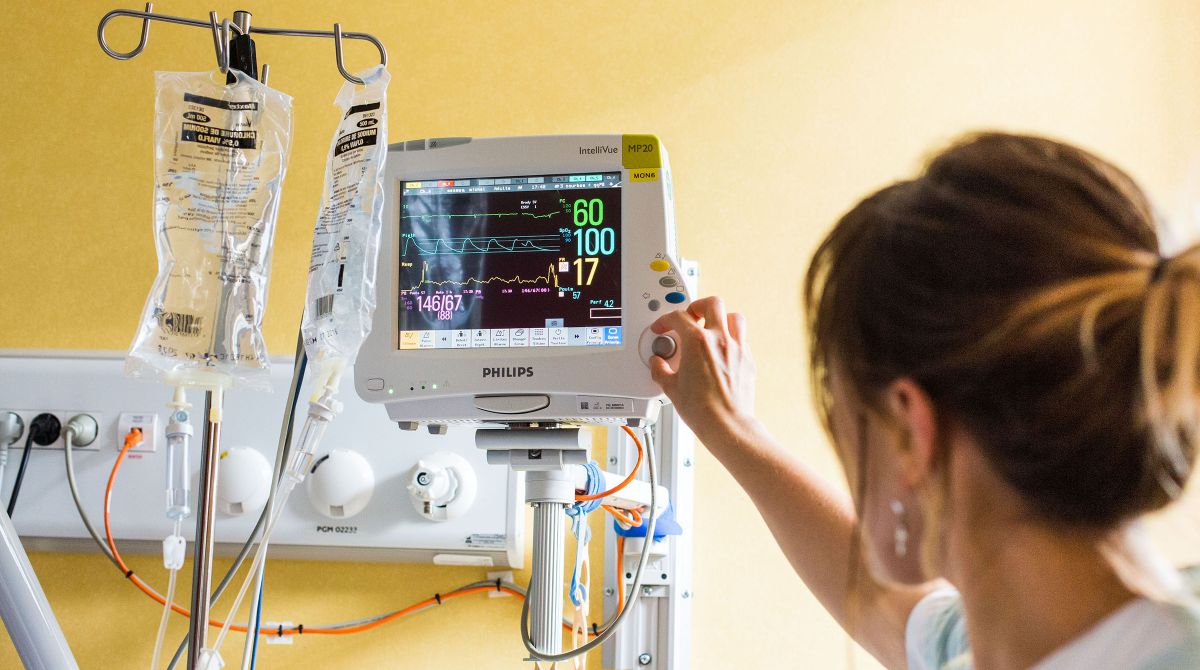
A study led by a Kingston University academic into the working lives of doctors and nurses in NHS intensive care units (ICUs) has revealed a workforce battling to cope with the critical demands of their jobs – leading to a crippling inability to switch off from life on the wards once their shift is over.
The study explores how ICU staff reflect on and think about their jobs when they're not in the workplace – and the impact such rumination can have on their mental and physical health. Almost 100 doctors and nurses from four NHS ICUs in the United Kingdom completed a questionnaire on burnout, ICU-related stress factors and general health.
Given the unpredictable and fast-paced nature of working in an ICU, it is widely acknowledged that doctors and nurses are under immense duress. However, according to the study's lead author, Dr Tushna Vandrevala, senior lecturer in psychology from the School of Social and Behavioural Sciences at Kingston University, these pressures can mount and intensify even when the shift is over.

The study also showed that 32 per cent of the sample felt their mental and physical health were deteriorating, an incidence known as psychiatric morbidity. There was an association between longer working hours and higher incidences of burnout and depression. "This is especially worrying as 43 per cent of our participants worked an excess of 40 hours a week," Dr Vandrevala suggested.
Dr Ben Creagh-Brown, a consultant physician at the Royal Surrey County Hospital in Guildford, and also a co-author on the study said the lengthy shifts were becoming more of a problem. "A nurse will do three or four 13-hour shifts a week," he added. "A doctor's week is variable, but it can be six days in a row of mostly 10-hour shifts, along with some 13-hour shifts. Both doctors and nurses working in ICUs work across day and night and while consultants can go home around 10pm, they are required to be on call throughout the night."
Dr Vandrevala concluded that the extensive working hours that ICU healthcare professionals undertook were hampering their ability to psychologically detach from work and unwind appropriately which could be indirectly affecting their patients. "Those working excessively may experience fatigue and decreased levels of efficiency," she warned. "Ultimately ICU doctors and nurses need greater periods of downtime and periods away from the wards to aid their mental and physical recovery from the intensity of their jobs. However, given the economic pressures facing the NHS, giving skilled professionals time off could lead to greater waiting periods for patients, which is something everyone is looking to avoid."
The study, which featured in the latest edition of the Journal of Intensive Care, highlights the importance of screening ICU healthcare practitioners for depression and burnout, and appropriately assessing if they can avoid thinking about their jobs negatively once away from the workplace. By identifying those who had a tendency to worry, NHS trusts could develop cognitive behavioural therapies and relaxation exercises for staff, which could help them cope more effectively with the emotional challenges they faced, she said. The cost and delivery of such a proposal needed to be thought out thoroughly but the health and wellbeing of ICU doctors and nurses could not be overlooked.
"Patient welfare will always be paramount - but we also have a duty of care to our healthcare professionals and must acknowledge the intensity of the unique and challenging job they do," she said.
- Find out more about studying Psychology BSc (Hons) and Psychology MSc at Kingston University.